How Strong is Ketamine Compared to Other Psychedelics? .Ketamine can be very powerful. While it’s less potent than other psychedelics in terms of the dose, the effects can become much more profound than many other psychedelic substances.
This drug is most comparable in terms of effects to PCP, but less potent and with a much safer profile.
Lower doses of ketamine are similar in their effects to MDMA, MDA, 2C-B, or 2C-E.
DXM, xenon gas, and nitrous oxide all work through similar mechanisms and have a similar dissociative effect.
The full dose of ketamine that leads to a K-hole experience is similar to DMT or salvia but feels subjectively different. A K-hole is usually dark (in more of a “low-light” way than evil or depressing), shadowy, and often involves the feeling of falling or being rapidly teleported to different locations.
How Ketamine Works
Ketamine is considered a “dirty drug”. This doesn’t mean the drug is toxic or poisonous — it refers to the specificity of the drug on its target receptors.
Ideally, a pharmaceutical targets one specific receptor to cause its effect. This makes its effects predictable and easier to study and understand. These drugs are precise and don’t cause any overflow effects on unrelated or irrelevant receptors.
Ketamine, on the other hand, is messy — it activates several different types of receptors, each with a different result. Ketamine stimulates some receptors and inhibits others.
This makes ketamine very difficult to study and understand. It’s also what makes this compound so useful for complex conditions like depression.
Ketamine has been shown to target the following receptors in the brain:
- Opioid receptors
- Blocks NMDA (glutamate) receptors at low doses
- Stimulates NMDA (glutamate) receptors at high doses
- Cholinergic receptors
- Dopamine receptors
- Adrenergic receptors
- Innate repair (HCN1 receptors)
- Sodium channels
1. Ketamine For Anesthesia
Ketamine is primarily used as an anesthetic agent in patients undergoing surgery or following a severely traumatic event. It’s more effective for blocking pain than opiate painkillers, which work by activating the opioid receptors in the spinal cord and brain.
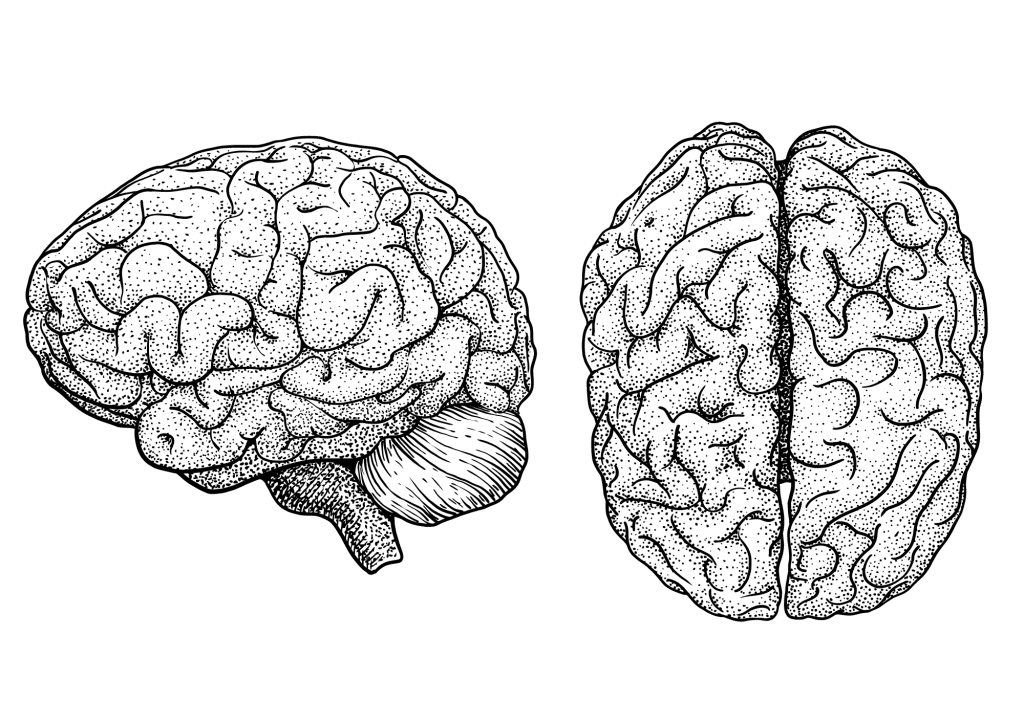
Ketamine works like most other dissociative analgesics — such as PCP, nitrous oxide, and DXM. They work by temporarily blocking the NMDA receptors — thus inhibiting communication between the cortex (the outer portion of the brain where higher thought occurs) from the thalamus. The thalamus is responsible for relaying messages from sensory information like pain, emotion, vision, and taste.
Studies have shown that ketamine owes most of its painkilling effects to its ability to block glutamate receptors (in lower doses) [2]. It also activates the opioid receptors, but to a much lower extent than typical opiate painkillers [3].
Other potential mechanisms for ketamine’s painkilling effects come from its ability to block the muscarinic and nicotinic receptors [4].
A meta-analysis exploring the outcomes of 11 clinical trials using ketamine for pain found it to be extremely effective for managing severe short-term pain but did not offer a good long-term solution for ongoing chronic pain [5].
2. Ketamine For Depression
Newer research (beginning in the early 2000s) shows that ketamine is also a powerful antidepressant. It works through mechanisms not offered by any other antidepressant on the market today. The effects of ketamine are fast-acting, exerting improvements in mood in as little as four hours after administration — even in treatment-resistant forms of depression.
Unfortunately, the effects of ketamine in this regard only last about seven days before another dose is required. It’s considered a third line of treatment for depression. Only when all other antidepressants have failed is ketamine prescribed to manage depression.
Only one ketamine product has been approved for use by the FDA — an isomer called esketamine, sold under the brand name Spravato®. This drug is made by the pharmaceutical company Janssen — a subsidiary of Johnson & Johnson.
How Spravato (and ketamine in general) works for treating depression is still not well understood. But here’s what we know so far:
Ketamine & Synapse Regrowth
Studies have shown that ketamine stimulates the growth of synapses [7]. This is an important finding because no other antidepressant that we know of can do this.
Chronic stress depletes the synapses in certain regions of the brain — especially the medial prefrontal cortex. This region is often implicated in the effects of depression. Researchers in the study gave mice ketamine and observed the formation of tiny spikes on the dendrites of the nerve cells. Spikes that survived for a few days after the treatment eventually formed into new synapses.
This effect is likely what causes the long-term benefits of using ketamine. However, this process takes a few days, so there must be other mechanisms that provide more fast-acting effects on depression.
The mechanism ketamine uses to cause this effect is extremely complicated and involves a cascade of effects [10, 11]. It’s believed ketamine has a greater affinity for glutamate receptors that are located on GABA interneurons, which are inhibitory neurons [12].
Ketamine blocks the effects of these neurons, which cause a downstream increase in glutamate. Excess glutamate activates postsynaptic AMPA receptors, which bolster the effects of BDNF and mTORC1 — which are ultimately responsible for the regrowth of synapses.
Unfortunately, there’s little evidence to suggest that ketamine has a lasting impact on depression. Most studies show that ketamine requires another dose every 2–3 weeks to maintain the antidepressant effects.
Blood Sugar Regulation
Ketamine has been shown to regulate blood sugar levels in regions of the brain associated with depression [6].
It’s not clear whether this has a direct benefit on depressive symptoms or if it’s a byproduct of other improvements in these brain regions.
Circadian Rhythm Regulation
Ketamine has been shown to improve the body’s ability to regulate the circadian rhythm [9]. Researchers are still seeking to understand whether these improvements come as a result of improved mood or if this effect contributes to the greater mood regulation instead.